The Optimal Diet , Atkins
, Atkins , South Beach
, South Beach , Paleo
, Paleo , Zone
, Zone … all have one thing in common: some degree of carbohydrate restriction.
… all have one thing in common: some degree of carbohydrate restriction.
Low, lower, lowest: does it matter?
There are 4 relatively large, randomized ‘diet-induced weight loss’ studies that all reported fairly comprehensive food intake and body composition data. The studies ranged in duration from 24 weeks to one year and included anywhere between 50 and ~300 overweight and obese participants.
In general, participants assigned to the low fat intervention were advised to restrict calories and fat whereas those assigned to low carb were told they could eat as much as they wanted as long as it wasn’t carbs.
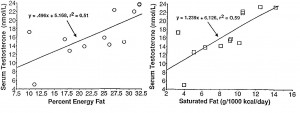
Your mileage may vary – but these studies cover a large number of subjects from a wide range of backgrounds, suggesting the results might be applicable across the board. Conclusion? the amount of body fat lost was much more strongly associated with the reduction in carbohydrates than calories. The only modestly surprising aspect was the magnitude… (see the figures below).
The four studies, in chronological order:
Brehm 2003: over the course of 6 months, those who consumed an average of 163 grams of carbohydrate per day lost 8.6 pounds of body weight while those who consumed 97 grams lost 18.7 pounds.
McAuley 2005: 24 weeks; those who ate 171 grams lost 10.3 pounds, while those who ate 133 grams lost 15.2 pounds, and those who ate 107 grams lost 15.6 pounds.
Maki 2007: 36 weeks; those who ate 186 grams lost 5.7 pounds, those who ate 131 grams lost 9.9 pounds.
Gardner 2007: 1 year – those who ate 138 grams lost 10.3 pounds, 181 grams lost 3.5 pounds, 195 grams lost 4.8 pounds, and 197 grams lost 5.7 pounds.
Continue reading →