Weight loss maintenance is not determined by calorie intake… or physical activity… but by The Laws of Energy Balance FTW!!!

Odd, the sensation I felt when reading this news release (gloating?). As reported at a meeting of the Obesity Society, results from the Utah Obesity Study of gastric bypass patients 2 and 6 years after surgery. By the 2 year mark, they lost over 100 pounds, or 36% of their starting weight (went from 296 to 189 pounds). Energy expenditure declined from 2201 to 1736 kcal/day. Food intake went from 2085 to 1638 kcal/day. (Hint: it’s no coincidence that energy expenditure and food intake declined to the exact same degree.) Physical activity and fitness levels increased.
By the 6 year mark, they still weighed 29% less than their starting weight. N.B. that’s an amazing level of success, it’s virtually unheard of in diet intervention studies. +1 for gastric bypass; -1 for nutrition.
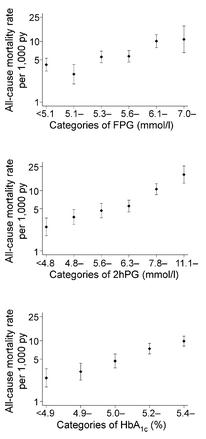
Here’s what piqued my interest: during the gradual increase from 189 pounds to 210 pounds, which occurred between years 2 and 6 post-surgery, the most significant factor associated with weight regain was not calorie intake or physical activity… it was metabolic rate. This represents another fail for “eat less move more,” and a win for the Laws of Energy Balance.
So what’s this got to do with The poor, misunderstood calorie?
what we know about metabolic rate:
1) It’s invisible.
2) Fructose vs. The Laws of Energy Balance (circa December, 2011): sugar-sweetened beverages can cause fat gain, not by providing excess calories, but by reducing metabolic rate.
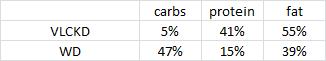
3) Holiday feasts, the freshman 15, and damage control (circa January 2012): overeating a high protein diet causes less fat gain than overeating anything else because it increases metabolic rate.
4) Missing: 300 kilocalories (circa July 2012): after losing weight, subjects assigned to the low carb diet maintained a higher metabolic rate than those on an isocaloric low fat diet.
“Eat less move more” is not the answer. But eating less sugar, more protein, and fewer carbs might be. Nutrition matters.
calories proper