Hint: “no”
DNL proper.
Lots of metabolism talk below, but first a brief intro. My “muse,” if you will.
Taubes’ recent article in the BMJ (Taubes, 2013; full text) generated some interesting feedback.
In the original article, Taubes basically re-states his philosophy on obesity. Nothing new. But one rebuttal by Cottrell got under my skin (Cottrell, 2013), and Taubes’ response was woefully inadequate.
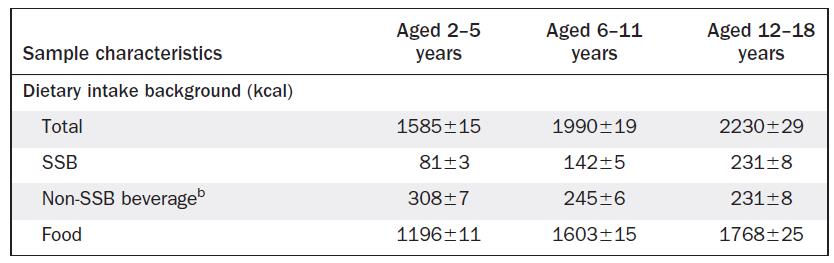
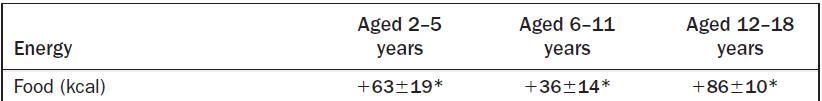
Cottrell [sic]: “A third incorrect assertion is that obesity can be attributed to the conversion of carbohydrate to fat. This is an unsatisfactory explanation of obesity, because this route is a minor pathway to depot fat in humans, even under conditions of substantial overfeeding of sugars to obese subjects. An unproved assumption is that the hypothetical diversion of carbohydrate energy into fat storage leaves the subject hungry, thus stimulating overeating.”
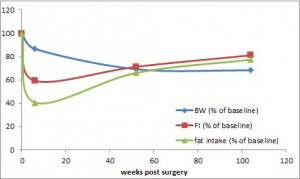
Cottrell set up a straw man and handily took it down. The primary mechanism whereby excess carbs contribute to obesity is via insulin’s effects on adipose tissue. Even if you’re eating very little fat, insulin will cause it to get stored. Insulin is very good at this – it is actually far more potent at stimulating fat storage than it is at stimulating glucose uptake (eg, Insulin vs. fat metabolism FTW). Cottrell’s straw man is that excess carbs themselves are stored as fat. This does not occur to any appreciable extent in humans. Here is why I believe that to be true, from one of most insightful and informative studies on the topic IMHO.