Warning: this post isn’t #Paleo Certified™. It’s more about convenience, choosing the lesser evil.
Quest Nutrition led the charge in low carb, high protein, fibre-rich bars. “Fibre-rich” is really the key in allowing a bona fide “low carb” bar with shelf-stability and decent texture. Sugar alcohols have also been used in some, but due to the high incidence of maltitol-induced GI discomfort, ymmv. But in general, you need one or the other to provide bulk and keep it together (except Epic Bars
led the charge in low carb, high protein, fibre-rich bars. “Fibre-rich” is really the key in allowing a bona fide “low carb” bar with shelf-stability and decent texture. Sugar alcohols have also been used in some, but due to the high incidence of maltitol-induced GI discomfort, ymmv. But in general, you need one or the other to provide bulk and keep it together (except Epic Bars , which use black magic).
, which use black magic).
For the most part, the new bars have basically copied Quest’s formula with some new flavors.
formula with some new flavors.
Disclaimer #1: I’m a whole foods guy. Not really #Paleo™, but when it comes to people’s actual lifestyles, I recognize convenience is a huge factor… and selecting the lesser evil is frequently the best option — eg, you can store a couple LC protein bars in your office, car, etc.; not so much with hard-boiled eggs or other protein-rich foods… and these options are WAY better than many other snacks or “fast-foods” out there.
Disclaimer #2: yeah, I keep a few of these bars in my office, just in case…
Quest recently switched from isomaltosaccharides to soluble corn fibre (SCF), which will likely impact GI effects. YMMV! Isomaltosaccharides are cool, but I’m not prepared to say they’re superior to SCF for everyone, in every #context (personally, for the ‘biome, I prefer brassicas, alliums, the gristly bits, galactooligosaccharides, et al.).
[it’d awesome if Bi2Muno would collaborate with one of these companies]
would collaborate with one of these companies]
In these n00bs to the protein bar market, some of the biggest differentiating factors are cost, net carbs, ratio of fibre to sugar alcohols, flavor profiles, etc.
With no further ado, here are the newcomers:
[or just skip to the chart at the bottom]
Continue reading →
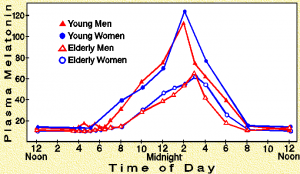
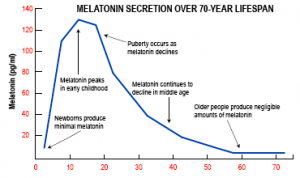
secretion happens at night (or at least that’s when it’s supposed to happen):