“please stop asking gurus how many carbs you need to optimize health”
An interesting paper came out recently by Zeevi et al. (2015), showing, in part, that we’re all unique snowflakes (in some contexts).
Mini-rant: this study is in line with a lot of my beliefs about individuality in human biology. We don’t know all the mechanisms, but we do know that some people respond better to some interventions than others. We learn a lot from studies on diet, light, sleep, physical activity, etc., but the findings rarely/never apply equally to everyone (and some people experience completely opposite effects; eg, see studies where individual data are reported). LIGHT exposure can improve sleep quality in some but cause agitation in others. Low carb diets can help weight loss in some people but low fat is better for others. Dairy, wheat, protein, the ‘biome, and fibre/resistant starch all fall into this category. Sleep ‘requirements’ vary by person, season, geography, etc., etc… there’s no QED answers in many of these contexts.
anecdote: some people say they’ve never had better blood glucose than when they were having a few servings of beans/legumes per week; others just report bloating & farts (no bueno).
End rant.
Background reading:
- The Atlantic ran a decent piece on this study (certainly more colorful than my take)
- Reddit AMA with some of the people involved in the study
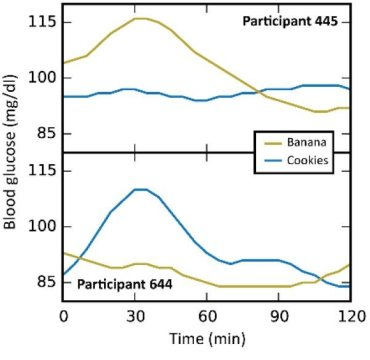
In this particular study (video summary below): they continuously monitored the blood glucose responses in 800 people to all of their meals for a week, including a variety of test meals. Main result: many different responses, even to the same foods! An oversimplified example: some people had smaller relative postprandial glucose excursions after 50g carbohydrate from rice compared to 50g carb from potatoes, and other people responded oppositely. And friggin’ tomatoes?!
Translation: need to move beyond recommending #IIFYM.
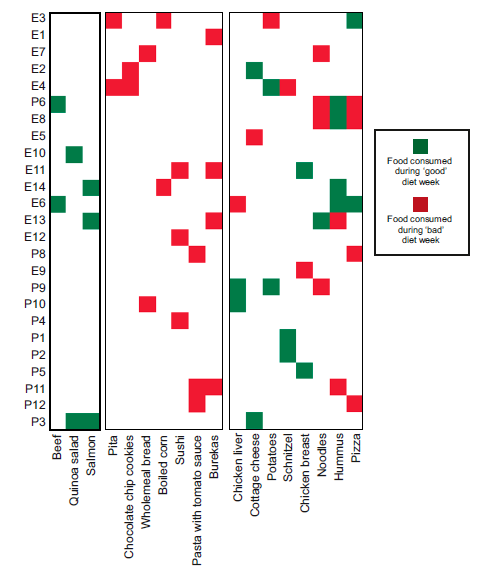
Some foods were universally well-tolerated [in this population] in the context of mixed meals, like quinoa and salmon; other foods did the opposite, like chocolate chip cookies and sushi. And lastly, some foods like cottage cheese and hummus were good for some people but others.
*In general, I don’t believe in labeling foods as categorically good or bad, which is pretty much confirmed by this study, but some patterns emerged wrt postprandial glucose excursions in this population…
#context
To make a crude study design to test these findings, they classified foods as good or bad based on blood glucose responses (for each person, on an individual basis), assigned them a diet consisting primarily of their good or bad foods for a week, monitored blood glucose, then crossed them over to the opposite foods.
Lo and behold, it worked!
N.B. all follow-up studies were in much smaller subgroups.
The most interesting part, in my opinion, was the divergent responses to the same foods. See the right side of the figure above (with mixed red and green boxes). These are the foods that worked for some people but not others (eg, taters were cool for subjects E4 and P9, but not E3).
Take-home message: there really is no one-size-fits all. Even seemingly healthy/non-offensive foods like liver, chicken, and taters caused opposite effects on blood glucose in different people (in the context of mixed meals). If you’re prone to postprandial hyperglycemia, you really can’t take other peoples “n=1” and hope it applies equally well to yourself (and definitely not IIFYM macro-based “n=1’s”). I don’t recommend obsessive blood monitoring for healthy people, but if you’re diabetic or need strict control over metabolites like glucose or ketones, then your own #context becomes critically important.
I really hope this study is stretched out into a few more publications, because they collected a TON of data, and other than the figure above, not many specifics were reported.
They also measured a slew of biomarkers and even analyzed the ‘biome (which was a big player)… and many of these things impacted how different people responded to specific foods.
Super-cool, right? It’s moving in the right direction, imo, along the lines of Chris Gardner’s work. They didn’t assess any potential correlations with sleep quality, season, or exposure to artificial light in this study, but they definitely matter, too.
correction: they measured sleep but didn’t report the results. Hopefully, this will appear in a future publication.
In conclusion, please stop asking gurus how many carbs you need to optimize health.
Video summary of this study:
For full access to all articles and much more (or if you just like what I do and want to support it), become a Patron! Five bucks a month for full access and there are many other options. It’s ad-free and you can cancel if it sucks 🙂
Also, I’m open to suggestions so feel free to leave a comment or email me directly at drlagakos@gmail.com.
Affiliate discounts: if you’re still looking for a pair of hot blue blockers, Carbonshade is offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE. TrueDark is running a pretty big sale HERE. If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.