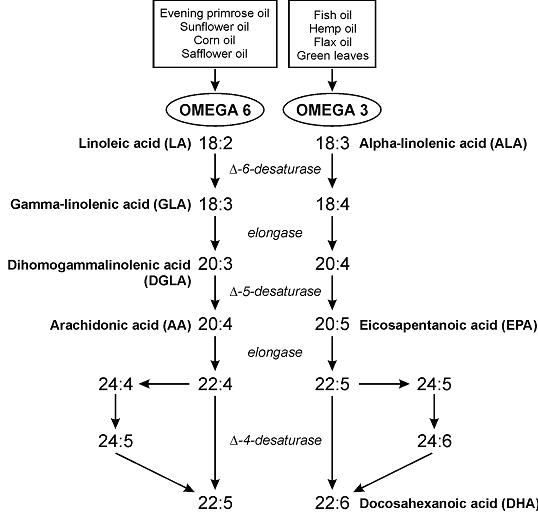
They are conditionally essential at best, only if docosahexaenoic acid (DHA) is lacking. We can’t synthesize omega 3 fatty acids, and indeed they do prevent/cure certain manifestations of “essential fatty acid (EFA) deficiency” (Weise et al., 1958), but DHA can do all that and more. Not that I recommend this, but a diet completely devoid of 18-carbon vege oil fatty acids will not produce EFA deficiency in the presence of DHA. (“vege,” rhymes with “wedge”)
The “parent essential oils” are linoleic acid (LA) and alpha-linolenic acid (ALA). The others, which I think are more important and the truly “essential” ones are eicosapentaenoic acid (EPA), arachidonic acid (AA), but mostly just DHA.
The first manifestation of EFA deficiency is dermatitis (Prottey et al., 1975). Some people say LA is necessary to prevent this, but it would be better phrased as “LA prevents dermatitis;” not “LA is necessary to prevent dermatitis.” All of the evidence suggesting LA is essential is in the context of DHA deficiency.
Technically, we can convert a bit of ALA to DHA, estrogen helps, testosterone doesn’t (women have better conversion rates)… and I’d speculate that the reverse is probably easier (DHA –> ALA).
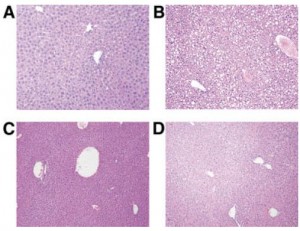
Exhibit A. Feeding mice a fat-free, high carbohydrate diet induces marked microvesicular and macrovesicular hepatic steatosis rather quickly (Alwayn et al., 2004).
A, chow (liver fat = 3.4%)
B, fat-free diet (24.1%)
C, supplemented with purified fish oils (7.2%)
D, supplemented with soybean oil (8.1%)
This study showed DHA was at least as good as vege oils in this context…
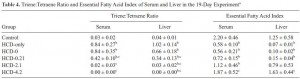
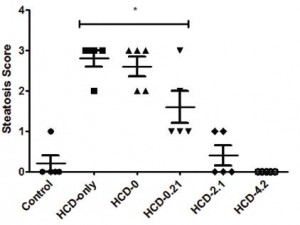
Exhibit B. EFA deficiency, not prevented by a diet with zero polyunsaturated fatty acids (PUFAs, eg, LA, ALA, DHA, etc.)… fat source was hydrogenated coconut oil (HCO), and EFA deficiency was fully prevented with 4% DHA + 0.2% AA.
HCD-only: fat-free, high carbohydrate diet, just like in exhibit A.
HCD-0: high carb diet supplemented with 5% HCO. It didn’t prevent EFA deficiency.
HCD-0.21: high carb diet supplemented with 0.2% DHA and 0.01% AA. It almost prevented EFA deficiency.
HCD-2.1: supplemented with 2% DHA and 0.1% AA. It worked.
HCD-4.2: 4% DHA and 0.2% AA. It worked.
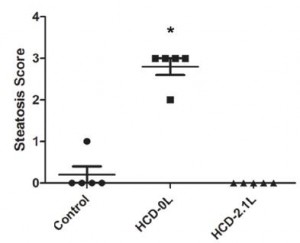
And, similar to exhibit A, steatosis was completely prevented when the diet contained at least 2% DHA (and 0.01% AA):
^^^that’s “acute.” Here’s “chronic:”
Now we’re getting somewhere. In the beginning, we thought LA and ALA were essential. Then we thought EPA, DHA, and AA. Now it’s just DHA and AA? …the top tier omega 3 and omega 6 fatty acids, respectively.
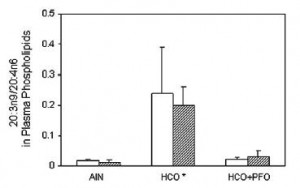
Exhibit C. AA isn’t even “essential” in a diet with no vege PUFAs, supplemented with EPA and DHA (Ling et al., 2012):
So, the diet needs either DHA and EPA or DHA and AA.
Exhibit D. DHA alone (Le et al., 2013)
MUAHAHAHAAA! (P<0.05)
Mice were fed, for 3-5 weeks, diets with 2.1% DHA plus AA, in ratios of 1:1, 5:1, 10:1, 20:1, 200:1, and 100:0. Yes, “100:0” means DHA alone. Do not pass GO! Do not collect $200. No vege PUFAs, EPA, or AA.
These were synthetic diets, with purified esters of DHA and AA. Clear biochemical evidence of EFA deficiency, completely abrogated by DHA.
a closer look:
I propose a new meaning for EFA: DHA.
I know LA and ALA do stuff in the body, and it’s virtually impossible to construct a diet with ZERO LA and ALA. But: 1) providing all of the fat as coconut oil and purified DHA comes pretty close; and 2) as mentioned above, your body can probably make some ALA/LA from DHA/AA. And there’s no need to avoid LA and ALA, I’m just saying it’s incorrect, or at least incomplete, to say they are the essential ones, when the long-term consequences of their deficiency pales in comparison to that of DHA. Don’t get me wrong, dermatitis sucks, but compared to impaired cognitive function and debilitating mood disorders, itchy skin is a walk in the park. (although evidence suggests it’s not an either/or situation; DHA prevents all of the above whereas LA only prevents dermatitis)
Remember Dr. Eades’ epic 2007 post about the Great Starvation Experiment? I’m pretty sure Sam Legg went nuts and chopped off his fingers in part because of DHA deficiency.
Part II: seafood > fish oil supps >> no DHA
DHA from seafood is likely more effective than that from supps, but supps aren’t worthless.
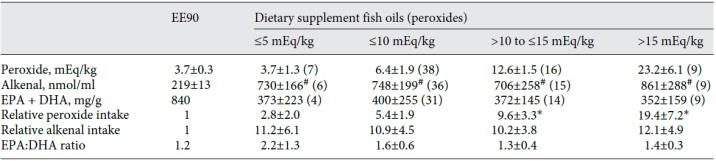
However, many fish oil pills contain unacceptable levels of potentially adverse peroxidation products. Out of 63 different products tested, Rupp and colleagues showed that many of ‘em did. Store in the fridge and discard if stinky.
Lastly, to get the most bang for your buck, it’s not as simple as “wild vs. farmed,” see the Fish Blog to see how DHA & contaminants vary by geography.
As Dr. Kruse has been saying, DHA must be present at the “sn-2” position (that’s basically the middle of a triacylglycerol or phospholipid). This is how DHA is present in seafood but not always in fish oil supps (eg, Litchfield 1968 and Ando et al., 1996). It’s not all-or-nothing, but it’s safe to say you’re gonna get more sn-2-DHA in seafood.
Why “sn-2?”
1) DHA is more stable in this position (eg, Wijesundera et al., 2008).
2) It’s more bioavailable here (eg, Christensen et al., 1995).
3) sn-2-DHA is more effectively incorporated into brain lipids (eg, Thies et al., 1994 and Lagarde et al., 2001). Again, it’s not all-or-nothing, but more is likely gonna get in your brain if you eat seafood.
Do not, under any circumstances, feel the need to supplement your diet with LA, ALA, or vege oils. Just eat seafood. DHA supps are negotiable (they’re better than nothing, imo).
If you like what I do and want to support it, check out my Patreon campaign!
UPDATED Affiliate links: still looking for a pair of hot blue blockers? Carbonshade and TrueDark are offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE.
If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.
Join Earn.com with this link.