This study was pretty interesting.
Three groups of women:
1) normal weight
2) gynoid obesity (stores more fat in hips & butt), defined by WC/HC < 0.85
3) android obesity (stores more fat in belly, which is rare in women), defined by WC/HC > 0.85
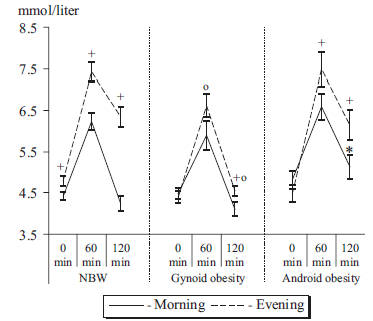
First, we get confirmation that insulin sensitivity (IS) is better in morning than evening. But then we get these interesting glucose tolerance curves:
Fat stored in your hips & butt is thought to be healthier than that stored in your belly region. This is confirmed here. Gynoid obesity, while exhibiting an attenuated AM/PM difference, was able to restore euglycemia by the end of the experiment at both time points. Ie, gynoid obesity selectively improved IS in the evening.
Android obesity, which is more nefarious than gynoid (also confirmed here), had a similar though not as robust effect in the evening but deteriorated IS in the morning.
One potential interpretation: it’s better to have a little extra fat stored in your hips and butt than to be lean or have belly fat. However, I have a qualm with that interpretation. Healthy people show a robust circadian difference in glucose tolerance. Just as insulin resistance (IR) is an accepted physiological phenomenon observed in some ketogenic dieters, I view this circadian difference, also, as physiological.