Jane Plain recently wrote a great article about the relationship between insulin, dietary fat, and calories. There are a lot of data on this topic, which collectively suggest: context matters!
For example,
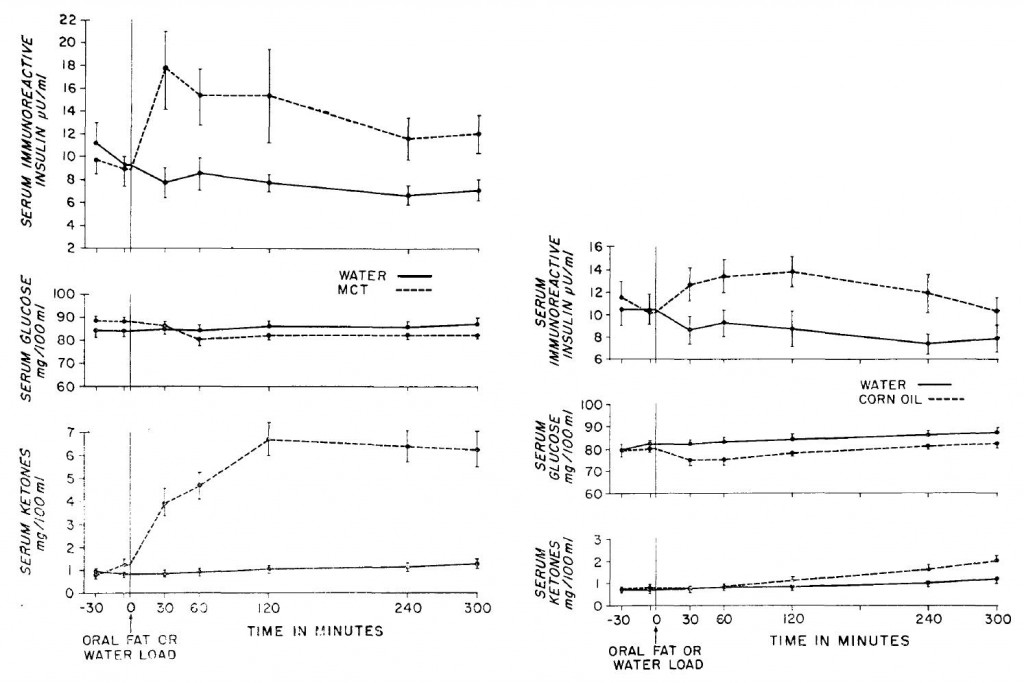
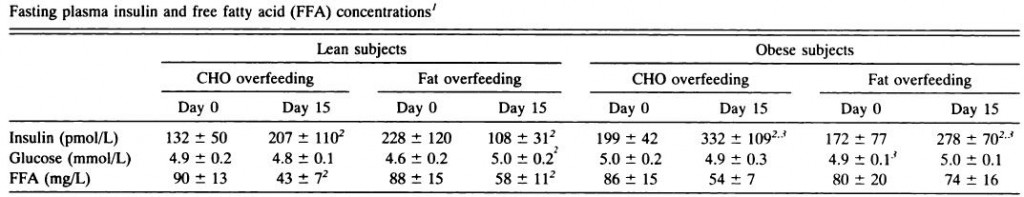
Insulin and ketone responses to ingestion of MCTs and LCTs in man. (Pi-Sunyer et al., 1969)
14 healthy subjects, overnight fasted; dose: 1g/kg.
In brief, MCTs are more insulinogenic than corn oil. But it’s not a lot of insulin. Really. Enough to inhibit lipolysis, perhaps, but that’s not saying much… & certainly not enough to induce hypoglycemia.
Stimulation of insulin secretion by medium chain triglycerides in patients with cirrhosis (McCullough et al., 1971)
100 grams glucose vs. 28.5 grams (30 mL) MCTs.
In this experiment, they gave about half as much MCTs as Pi-Sunyer and saw no insulin response in healthy subjects but a doubling of insulin in cirrhotics; still, however, this wasn’t enough to budge blood glucose. Note that after 100 grams of glucose, insulin increased 6-7x. That’ll leave a mark.
N.B. these aren’t direct comparisons; I know this. Context still matters.
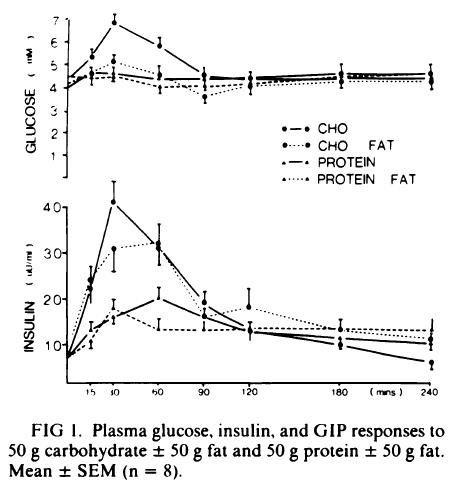
The coingestion of fat on the glucose, insulin, and GIP responses to carbohydrate and protein. (Collier and O’Dea, 1983)
Simple enough: healthy young subjects fed a boiled potato or veal, with or without butter. Carbs stimulate insulin the most; this is blunted by dietary fat. Protein stimulates less insulin; this, too, is blunted by dietary fat. The insulin AUCs were pretty much unaffected by dietary fat.
Also note that 50 grams of carbs increase insulin ~5x (significantly more than corn oil and MCTs). For other patient populations or different foods, check HERE & HERE.
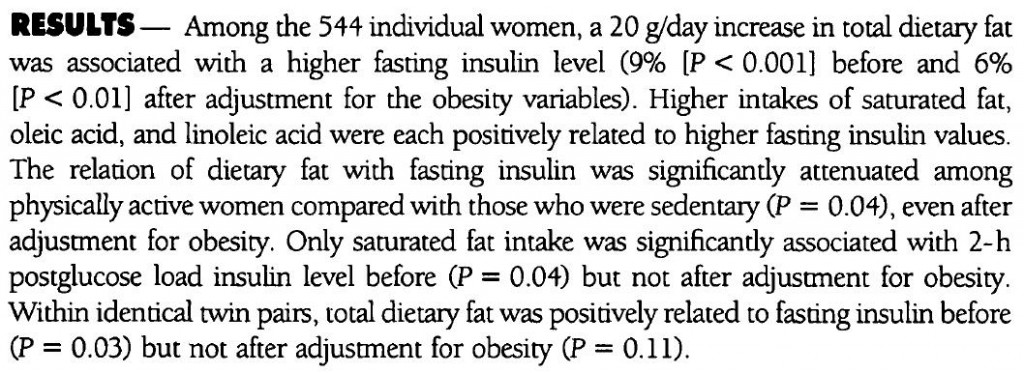
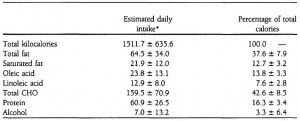
One of the studies cited by Jane: Usual dietary fat intake and insulin concentrations in healthy women twins. (Mayer et al., 1993)
Most of the correlation was attributable to body weight, but even after controlling for a variety of potential confounders, there was still a relationship between dietary fat and fasting insulin (but not fed insulin).
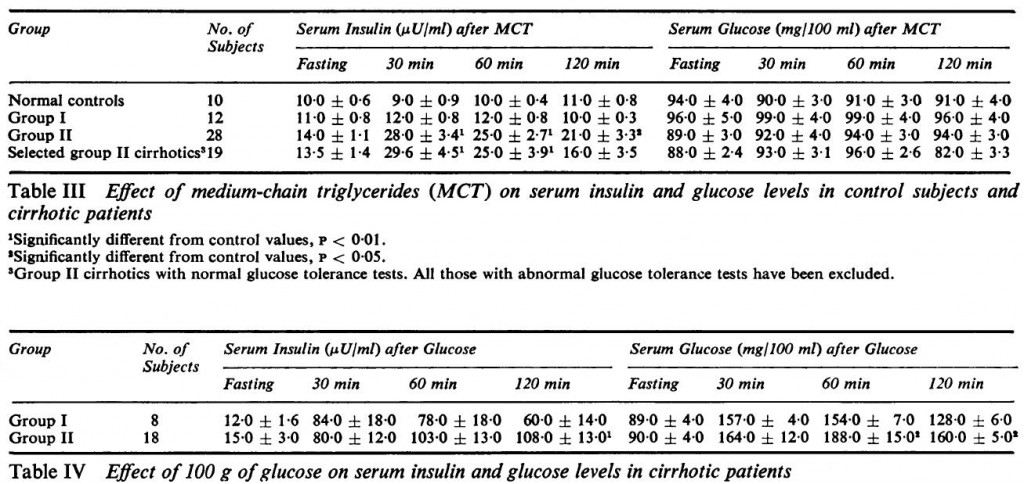
Fat and carbohydrate overfeeding in human: different effects on energy storage (Horton et al., 1995)
When in positive energy balance, excess dietary fat is insulinogenic in obese people, but carbohydrate overfeeding is still way more insulinogenic (in everyone).
Lastly,
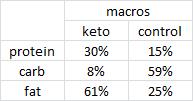
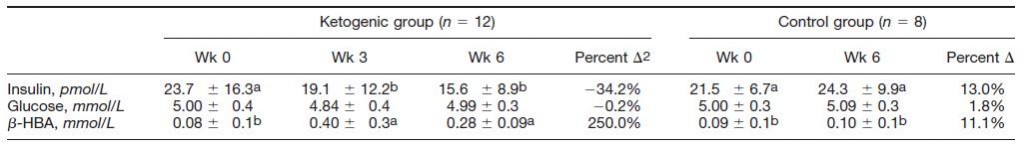
A ketogenic diet favorably affects serum biomarkers for CVD in normal weight men (Sharman et al., 2002)
Much higher fat intake (157 vs. 50 grams), but much lower insulin levels. Context matters! #EnergyBalance
Conclusions:
Keto-warrior dieters, 1-meal-per-day, etc. (unless you’re losing weight): insulin. Even if it’s 100% fat, there will be some insulin secreted (Pi-Sunyer). Probably enough to inhibit lipolysis, but not much else. If you’re lean or losing weight, and eating a few LC meals throughout day, insulin levels will remain low (Horton).
Fat blunts the insulin response to meals; even if the additional calories aren’t accounted for. In the Collier study, 50 grams of carbs (200 kcal) induced more insulin than 50 grams carbs + 50 grams fat (650 kcal).
If energy surplus and overweight (or post-obese, as per Jane’s analysis [I think]), then it’s also likely that higher fat –> higher fasting insulin (Mayer & Horton).
If you’re in relative energy balance, and not ingesting 2000 Calories all at once, then the old rules apply: low carb = low insulin (Sharman).
LCHF works well in obesity primarily because of the spontaneous reduction in food intake; insulin levels and body fat decline.
Context matters!
If you like what I do and want to support it, check out my Patreon campaign!
UPDATED Affiliate links: still looking for a pair of hot blue blockers? Carbonshade is offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE.
If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.
Join Earn.com with this link. Get free magical internet money!