But first, a brief primer. In red.
“The glucose muscle-sparing effect of fat-derived fuels”
or, the Randle Cycle 2.0. it’s like a course in life enhancement.
Part I. Intermediary metabolism
The glucose-fatty acid cycle
The Randle Cycle, as originally proposed, states that fatty acid oxidation inhibits glucose oxidation. This is good because during starvation, every tissue than can survive on fatty acids instead of glucose should do so, sparing as much precious glucose as possible for the brain.
The glucose-sparing effect of fat-derived fuels
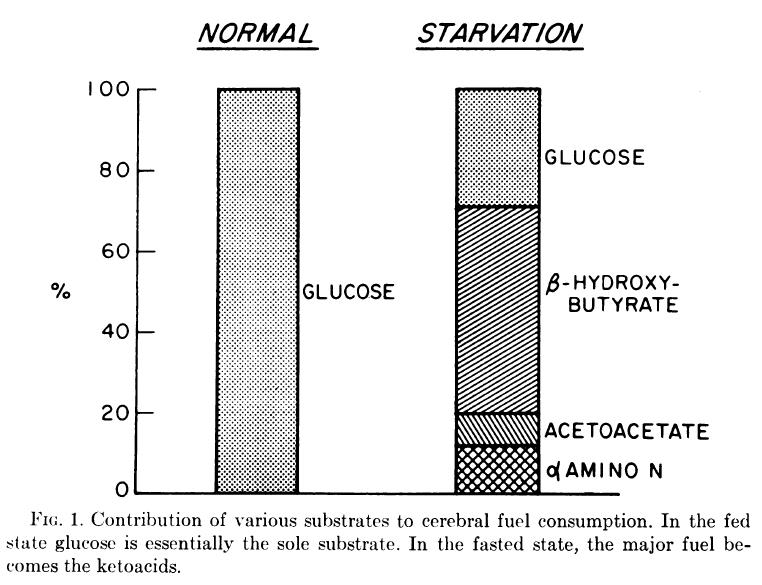
A critical vital horcrux to this is in the oh-so-humbly-disguised phrase “fat-derived fuels.” The fat-derived fuels are ketones, and they are rescuing the brain from starvation (ie, neuroglycopenia); they do so by supplementing glucose as a fuel source. Ketones are good at this; many tissues are happy to oxidize ketones when they are available.
The glucose muscle-sparing effect of fat-derived fuels
Ketones are derived from fat. During prolonged starvation, glucose comes from skeletal muscle amino acids (eg, alanine). Ketones spare glucose. Thus, ketones spare muscle. QED.
Part II. The brain
Even the brain loves ketones! Who it loves more is unknown (glucose or ketones), but what is known is that when blood ketones get high enough, the brain will happily utilize them for fuel. Happily. Whether or not it was known by Randle at the time, the glucose-fatty acid cycle could work just as well as the muscle-n-ketone cycle.
End background. Enter best keto study. EVER.
Resistance to symptomatic insulin reactions after fasting (Drenick, Alvarez, Tamasi, and Brickman, 1972)
Starved-obese but otherwise healthy men who hadn’t had anything to eat for two months. TWO months. Down ~73 pounds, and what do they get? jabbed by a syringe filled with insulin! (p.s. <– read that link if you’ve got the time)
Flashback two months.
A group of obese but otherwise healthy men volunteer for a weight loss study, and they undergo an insulin tolerance test. ~0.2 U/kg insulin injected, and plasma insulin shoots up from 30 to about 1000 mU. As expected, blood glucose plummets: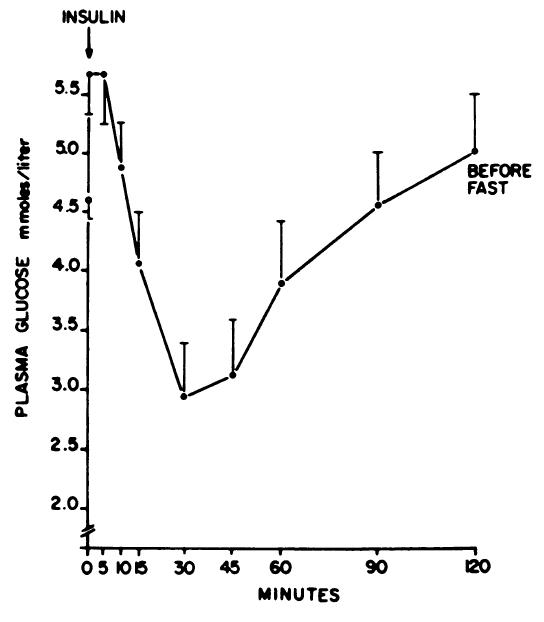
and surprise, surprise, they experienced: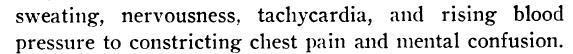
Ie, clinical hypoglycemia.
Then oddly enough, the men agreed to stay in the study, which consisted of two months of total starvation. They lost 73 pounds on average; and what do they get for this astounding accomplishment?? jabbed again! 2 months starvation, then another insulin tolerance test. Blood glucose started out a little lower than pre-fasting (not surprising), and it went down a little further: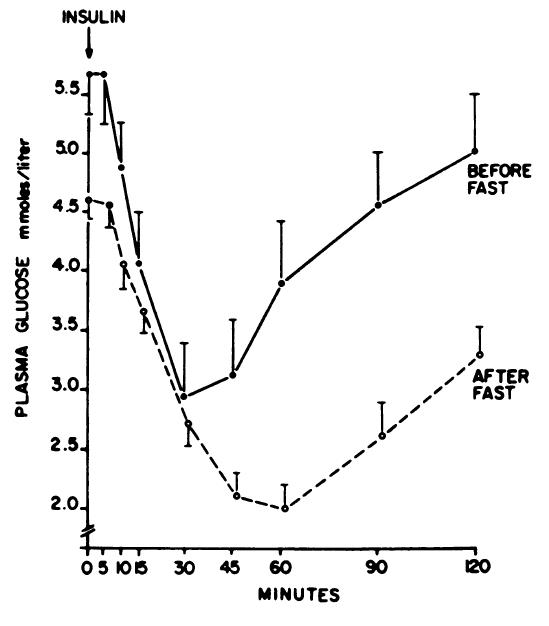
After the fast, the same nine subjects had no insulin reactions.
AFTER THE FAST, THE SAME NINE SUBJECTS HAD NO INSULIN REACTIONS.
Blood glucose at 2 mM, or about 36 mg/dL, and absolutely no clinical symptoms whatsoever.
what is known is that when blood ketones get high enough, the brain will happily utilize them for fuel. Happily.
Prior to ketosis, if you deprive the brain of glucose, you get shaky nervous sweaty confusion. During ketosis, the brain is all like: “whatever sugar, I don’t need you.”
all because of THIS
After two months of starvation, you’re right about here: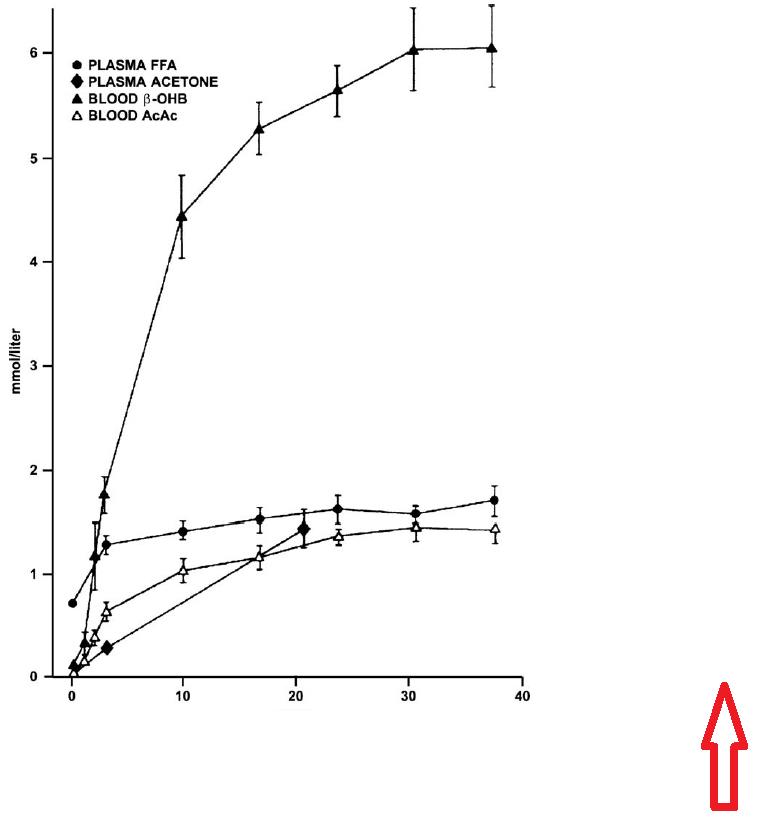
when blood ketones get high enough, the brain will happily utilize them for fuel. Happily. (see that line at the very tippy top of the graph above? yeah, that’s ketones)
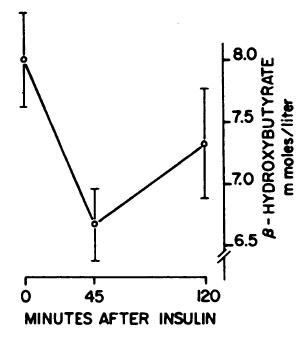
Even after getting jabbed with insulin, their ketones were above 6 mM (which is “high enough” by any definition):
sooo….
Starvation and survival (Cahill and Owen, 1968)
In NORMAL, take away the glucose and get all shaky nervous sweaty confusion. In STARVATION, however, take away that paltry contribution of glucose and everything runs A. O. K.
next time someone says you need to eat carbs to fuel your brain…
Consults are open, contact me if interested: drlagakos@gmail.com
If you like what I do and want to support it, check out my Patreon campaign!
Affiliate links: Still looking for a pair of hot blue blockers? TrueDark is offering 10% off HERE and Spectra479 is offering 15% off HERE. If you have no idea what I’m talking about, read this then this.
Join Binance and get some cryptoassets or download Honeyminer and get some Bitcoins for free!
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.
Join Earn.com with this link.