update: I learned a new trick. If you haven’t been receiving the regular updates to which you subscribed, it’s probably due to spam filters. Cure: find the update in your spam folder and reply to it. You don’t have to write anything, but the mere act of replying somehow tells your spam filter that the email wasn’t spam. It works for gmail, fwiw.
I [still] predict public approval of dietary fat will come along at a snail’s pace, and it won’t be a pan-approval of dietary fat at all. Instead, it will be selective approval of individual fatty acids. First, it was the medium chain fatty acids found in MCTs and coconut oil
. Then, it was the fish oil fatty acids
eicosapentaenoic and docosahexaenoic acids (EPA and DHA, respectively). Then, palmitoleic acid. Corn and soybean oil, on the other hand, are being appropriately recognized as bad. The utter hatred and fear of saturated fats is starting to wane, and we might even see a transition back to lard
before I die (circa 2113). But today’s post is on another topic: trans fats, oxidized fish oils, and dairy fat.
What happens when dietary fat is abused?
If it’s saturated fat, nothing. Saturated fat can be stored indefinitely and is invulnerable to attacks which would destroy polyunsaturated fat. Polyunsaturated oils, on the other hand, have a glass chin. With a little exposure to heat, light, or oxygen, they turn into trans fats, hydroperoxides, and aldehydes (oh my!). Imagine a piece of salmon that is a few days old or has been frozen and thawed one too many times… that horrific fishy odor is most likely a product of the very long chain polyunsaturated fish oil fatty acids. Or imagine some crisp fast food French fries… every time a new batch of frozen fries go into the deep fryer, the trans fat content of the oil and fries goes up dramatically- trans fats don’t smell, but if they did it would probably smell like delicious. 
A report following-up on NY’s trans fat ban was published in JAMA.
Change in trans fatty acid content of fast-food purchases associated with New York City’s restaurant regulation (Angell et al., 2012)
I wouldn’t say “NYC’s trans fat ban made people healthier” … but the media did. Their threshold for “healthier” is considerably lower than reason should permit. Other journalists went on to describe “Why NYC’s trans fat ban is good for the heart” – an equally wild interpretation of the new study.
In brief, the study authors looked at thousands of fast food receipts and calculated the amount of trans fats per meal between 2007 and 2009. Over the course of about 2 years, the amount of trans fats decreased from 3 to 0.5 grams. But that in no way means people are eating fewer trans fats; indeed, they might be, this just isn’t how you prove it. Why not? Maybe a bunch of people trying to get healthier switched from fast food fries to salad, but also opted for what they thought would be other healthy choices like microwave popcorn or low fat muffins. Both of these things would easily compensate for the 2.5 grams… and unfortunately, these choices are not unlikely for “a bunch of [misled] people trying to get healthier.”
Point #1. I hate to nit-pick, but I also hate scare tactics.
The authors tried to impress upon us the grave importance of reducing trans fats by saying [sic]: “An increase of just 2% of total energy intake from trans fat increases the incidence of coronary heart disease by as much as 23%.”
Only 2% = a whopping 23%!
They make it sound like your risk of dying is increased just by walking past a restaurant that serves anything made with partially hydrogenated vegetable oil. Here’s the thing about that “2%” – it’s about 300% higher than the average trans fat intake… in other words, it’s like quadrupling your trans fat intake; a whopping increase – so a whopping 23% increase in CHD is not so disproportionately high. And the trans fats in question are present in junk food, baked goods, and empty calories.
So picture all the foods you ate for breakfast, lunch, dinner, and any snacks. Divide them into 3 groups: whole foods (meat, vegetables, etc.), mixed foods, and empty calories (chips, fries, doughnuts, muffins, etc.). Now imagine a diet where you’re eating 3x more of those in that last category, at the expense of the others. Now instead of eggs, cereal, and a doughnut for breakfast, it’s 2 doughnuts. 3 single serve bags of chips throughout the day. 2 pieces of cake for dessert (and 2 more for “seconds”). In other words, it’s not as easy as walking past a restaurant that serves anything made with partially hydrogenated vegetable oil to quadruple your intake of trans fat. It’s a completely different lifestyle and I’ve got no doubt that it could be associated with a 23% increased risk for coronary heart disease, but it’s not like the picture painted by the authors. It’d look more like this:
Point # 2. Not all trans fats are created alike.
In general, industrial trans fats (the bad kind) come from vegetable oils used in baking and processed foods. Ruminant trans fats, on the other hand, are naturally present in meat and dairy. It’s only the former about which we need to be worried (eg, Bendsen et al., 2011; Ganguly and Pierce, 2012). Besides their association with heart disease, industrial trans fats intake is correlated with increased visceral fat, something not seen with ruminant trans fats (Hansen et al., 2012). But admittedly, this point is not that important; when the news media reports on the bane of trans fats, they are usually referring to the industrial trans fats that generally accompany sugar-rich, highly processed, empty calorie-containing foods… which is correct (see picture above).
Moving on (non-sequiter, remember?),
is stinky fish toxic?
When fatty fish intake was shown to be superior to the major cardiovascular drugs in preventing all-cause mortality, I felt a warm sensation of gloating. But a recent study on the impact of oxidized or otherwise “damaged” fish oil fatty acids had the potential to thrown a monkey wrench in the gears.

Oxidised fish oil does not influence established markers of oxidative stress in healthy human subjects: a randomized controlled trial (Ottestad et al., 2012)
Theory: Fish oils + heat, light, oxygen = hydroperoxides + aldehydes
Hydroperoxides + aldehydes = bad
Healthy non-smokers were given 8 grams of regular fish oil, oxidized fish oil, or sunflower oil for 7 weeks. For the first 3 weeks, all food was provided by the researchers; for the next 4 weeks, everybody went back to normal diets.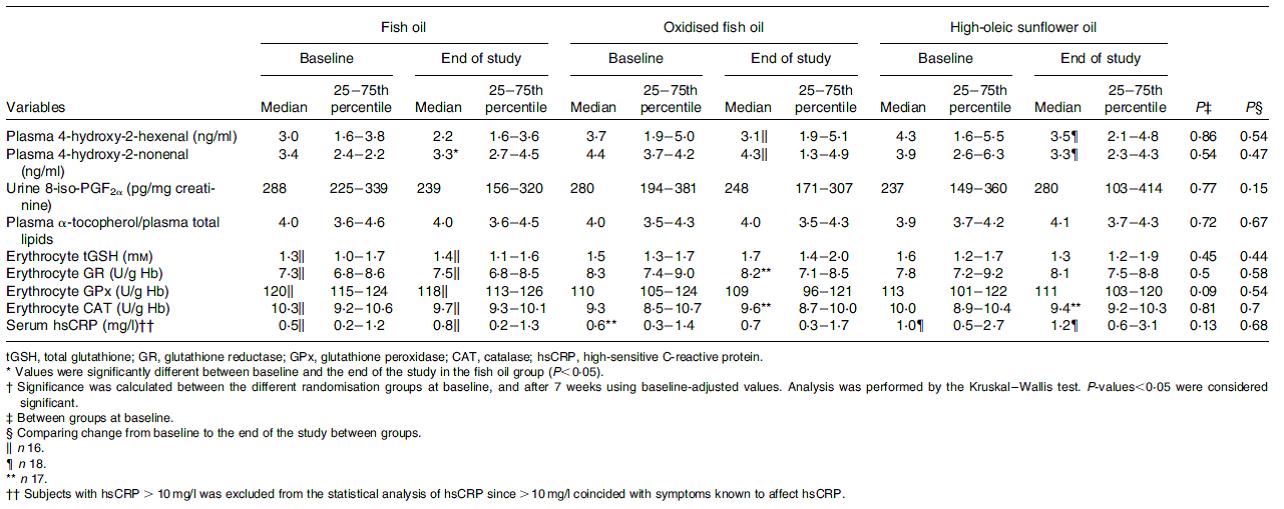
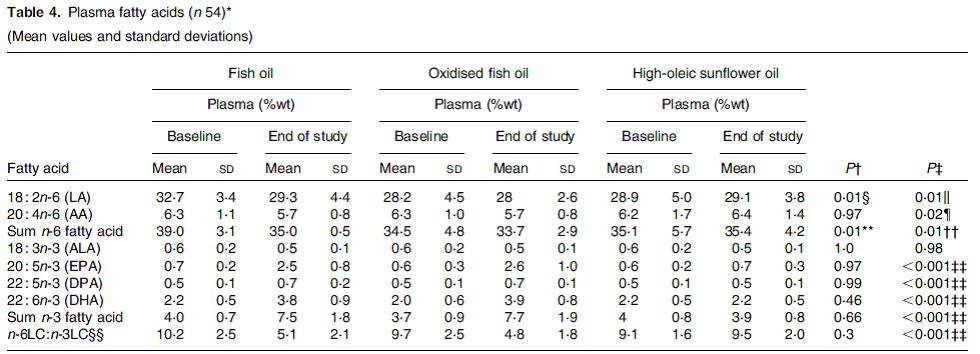
Don’t bother straining your eyes. There were no differences in any oxidation markers between the groups. And there was nothing fishy with the supplements; they produced the expected changes in plasma fatty acids. Ie, when people took pills containing a lot of EPA & DHA, a lot of EPA & DHA appeared in their blood:
Granted, this study was looking at intermediate markers, or surrogates for the disease process that oxidized fish oils are theorized to promote. Maybe it was the wrong markers? Alternatively, despite the foul odor, maybe stinky fish just isn’t bad for you.
Dairy fat
Ingestion of whole fat dairy, with all of its ruminant trans fats, is associated with lower adiposity (Kratz et al., 2012). And in the longest crossover study I’ve ever seen (6 months!), an intervention aimed at increasing the consumption of high fat dairy improved working memory better than low fat dairy in overweight and obese adults (Crichton et al., 2012). Food for thought.
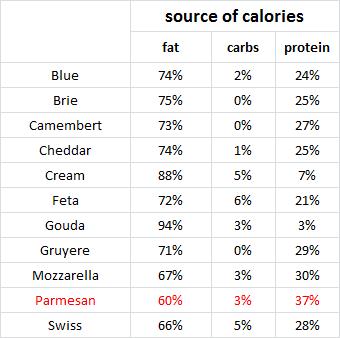
Parmesan, the protein bar of cheese: