but they actually get it right this time. Big HT to George Henderson for bringing this ms to my attention.
In Nutrition Disinformation, Part I, the Mediterranean diets employed by Estruch & colleagues were discussed. The study subjects’ need for antidiabetic drugs, insulin, and anti-platelets all increased over the course of 5 years. The media and even the authors themselves reported the opposite, touting the benefits of Mediterranean diets. Thus begat the Nutrition Disinformation series.
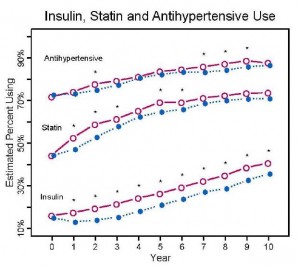
Nutrition Disinformation 2.0 was a follow-up to an older post on the Look AHEAD study, when the results were finally published. The intensive lifestyle intervention consisted of a pharmaceutical-grade low fat diet (ie, LFD + a little bit of Orlistat), and exercise. By the end of 10 years, medication use was modestly lower in the intensive lifestyle group compared to controls, but it was markedly increased from baseline. Therefore, I deemed it egregious to say their intervention was “healthy.” In the context of Nutrition Disinformation, “healthy” means you’re getting better. The need for insulin, statins, and anti-hypertensives should decline if you’re getting better.
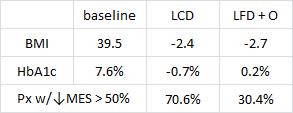
In part 3 of the series, Yancy must’ve been following the Nutrition Disinformation series 🙂 and decided to conduct a subgroup analysis on the patients in his previous low carb vs. low fat + Orlistat study. Weight loss was roughly similar, but all other biomarkers improved more on low carb. In the new publication, Yancy analyzed data selectively from the diabetic patients in his original study to generate a “Medication Effect Score (MES).” MES is based on what percentage of the maximum dose was a patient given, and adjusted for the median decline in HbA1c experienced by patients on said drug. A bit convoluted, but I’m on board (at least tentatively).
Two diets with different HbA1c and antiglycemic medication effects despite similar weight loss in type 2 diabetics (Mayer et al., 2013)
The low carb diet was <20 g/d carbs & unrestricted calories. Low fat was <30% fat (pharmaceutically enforced with Orlistat) and a 500-1000 kcal restriction.
The reduction in BMI of diabetic patients on a calorie restricted pharmaceutical-grade low fat diet (LFD + O) was modestly greater than those on a calorie unrestricted low carb diet. However, the effects of LFD + O on HbA1c went in the opposite direction DESPITE the fact that this group was taking more antidiabetic medications. Other subjects went off their antidiabetic meds, which would be expected to increase HbA1c and blood glucose levels, but this didn’t happen. Why? Because they were fortunate enough to be assigned to what the Nutrition Disinformation series classifies as a “healthy” diet… To be clear, the definition of “healthy” I’m using is this: getting better. If meds went down but metabolic calamity ensued, then it wouldn’t be a “healthy” diet. 70% of people on LCD were able to achieve a reduction in MES by half compared to 30% on LFD+O despite similar changes in BMI.
Whether or not the MES catches on, this measure or one like it should be applied to every nutrition intervention study – body composition is important, but so is this.
If medication use in subjects on both diet A and diet B increase by the end of the study, but on diet B it increases to a greater extent, then it shouldn’t be said that diet A is “healthy” because it resulted in lower meds than diet B… or at least medication use should be included in the abstract (so as to not mislead the media). Maybe it’s a high bar to set, but I don’t think so. What does a healthy diet look like?
Hint: not this –>