People have been fermenting food for a long time, all over the world. Different cultures have different traditional fermenting techniques for various foods and beverages (eg, Bell et al., 2017). Many things, ranging from grapes, milk, and cabbages, even meat and fish. For all intents and purposes, it’s practically universally viewed as a beneficial and healthful practice …
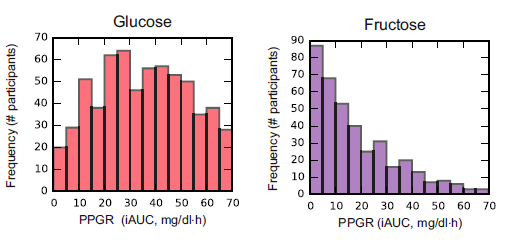
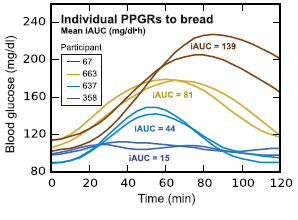
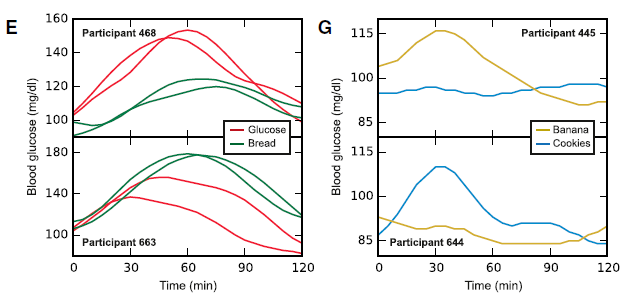
Maybe it’s just because a robust ‘biome lowers the sugar content of your diet! LOL jk I’m sure it’s far more complex than that.
Also, the shelf-life of most ferments is forever, so when the zombie apocalypse happens, it’s a good skill to have.
Part 2. Project FermenTRP
I started down this rabbit hole because the TRP theory of muscle cramps is interesting. And, well, I got carried away LOL .
The idea of a “superfood” is kinda silly, but virtually all TRP agonists are found in so-called superfoods. Fermenting is cool, too, so I decided to combine the two because why not
[I know, I know, photography isn’t my specialty]
#torched
Torching habanero peppers does not lessen the burn. To be honest, I’d go with a WAY less hot pepper. And combine with other TRP activators. For synergy. Or something.
The TRP-theory, in brief:
An interesting theory on the treatment of muscle cramps
Herbs, spices, TRP receptors, and pain
TRP channels in the treatment of muscle pain & cramps
Here are some of the more common sources of TRP agonists in the literature:
Hot Peppers (capsaicin) (doesn’t have to be habanero) (DO NOT USE HABANERO)
Involvement of thermosensitive TRP channels in energy metabolism (Uchida et al., 2017)
Targeting nociceptive TRP channels to treat chronic pain: current state of the field (Moran and Szallasi, 2017)
Peppercorns (piperine)
Activation of TRPV1 and TRPA1 by black pepper components (Okumura et al., 2010)
Ginger (gingerols)
Effects of ginger and its pungent constituents on transient receptor potential channels (Kim et al., 2016)
Garlic (allicins & sulfides)
The pungency of garlic: activation of TRPA1 and TRPV1 in response to allicin (Macpherson et al., 2005)
Diallyl sulfides in garlic activate both TRPA1 and TRPV1 (Koizumi et al., 2009)
Intragastric administration of allyl isothiocyanaate increases carbohydrate oxidation via TRPV1 but not TRPA1 in mice (Mori et al., 2011)
Cinnamon (cinnamonaldehyde)
Effects of TRP channel agonist ingestion on metabolism and autonomic nervous system in a randomized clinical trial of healthy subjects (Michlig et al., 2016)
Mustard & Wasabi (isothiocyanates, I think)
The capsaicin receptor TRPV1 is a crucial mediator of the noxious effects of mustard oil (Everaerts et al., 2011)
Thermosensitive TRP channels and brain function (Tominaga, 2016)
Cloves (eugenol)
Oregano, thyme, and clove-derived flavors and skin sensitizers activate specific TRP channels (Xu et al., 2006)
There are many more, but those are just some of the ones that made it to part 3.
For the rest of this article and much more, head over to Patreon!
Three bucks a month for access to all articles and there are many other options. And it’s ad-free.
If you’re on the fence considering it, try it out, you can cancel at any time! Also, there is a limited number of positions remaining at the $3 level.
Lastly, I’m open to suggestions; please feel free leave a comment or email me directly at drlagakos@gmail.com.