T.S. Wiley wrote a lot about the protein-rich breakfast; here’s my understanding of her take on it.
N.B. I highly recommend her book, Lights out: sleep, sugar, and survival.
Quotes are mainly taken from the text. I’ve tracked down some of the cites; the rest are in the back of the book, albeit somewhat unorganized :/
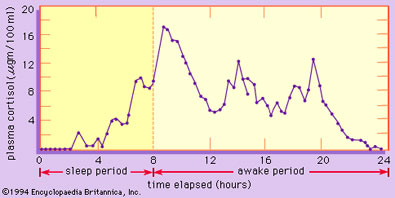
Part 1. We naturally have a cortisol spike first thing in the morning, known as the Cortisol Awakening Response (CAR). This peak, which can be screwed up by artificial light at night or a big evening dinner, helps support morning light-induced dopamine.
Dopamine is great, but may induce impulsivity if it’s unfettered.
Enter: the protein-rich breakfast. It provides tryptophan and a bit of insulin to promote serotonin synthesis (eg, Manjarrez-Gutierrez et al., 1999).
Not enough serotonin to make you crazy, just enough to balance the dopamine = impulse control.
~ circadian balance achieved ~