I walk a lot. Usually after meals; sometimes for sunlight & exercise, other times just because it’s a habit and I like doing it. Sometimes even twice a day (eg, after breakfast and lunch).
But seriously, it’s way healthier than I thought. This has been in-and-out of the news a few times over the years, but I was always like, “duh,” until I finally looked at the numbers. In some cases glucose & insulin excursions are down 20, 30, even 50%! (mostly depending on the distance covered, but also speed) (but mostly distance).
LOL there are like, a million studies titled “breaking up prolonged sitting improves everything” haha
And since the effects are acute, a lot of well-controlled RCTs — the flipside of that is you have to do it every day… my opinion is that total glycemic exposure over the course of your life is an important metric (more on the MOA below); and with the rise of continuous glucose monitoring systems, this will be proven true.
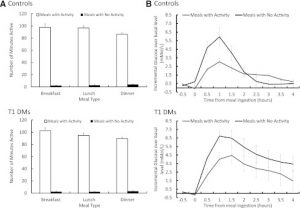
Exhibit A. The biggest intervention (VERY long walks, 5-6 hrs/d), but most profound results (Manohar et al., 2012)
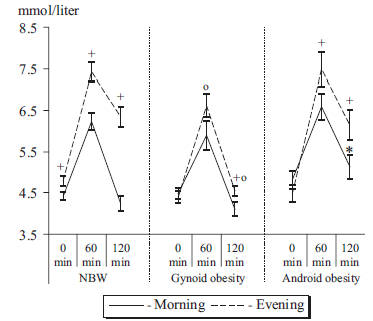
Exhibit B. Prolonged sitting vs. a 30-minute walk vs. 1.5 minutes walking every 30 minutes throughout the day (Peddie et al., 2013). Both of these interventions are very doable, imo.
In this study, the total daily exposure was 49, 47, and 30 mM / 9 h. 90 seconds of walking every 30 minutes cut glucose by almost half. HALF. Insulin also dropped precipitously. If you work a sedentary job, MAKE TIME FOR THIS. EVERY DAY. GO NOW.
For the rest of this article (it’s good, I promise!) and much more (or if you just like what I do and want to support it), head over to Patreon! Five bucks a month for all access and there are many other options. It’s ad-free and you can cancel if it sucks 🙂
Also, I’m open to suggestions, so please don’t hesitate to leave a comment or contact me directly at drlagakos@gmail.com.
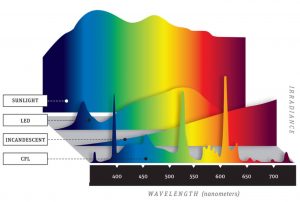
Affiliate discounts: if you’re still looking for a pair of hot blue blockers, Carbonshade is offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE. TrueDark is running a pretty big sale HERE. If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.