There are a lot of mysteries involving melatonin, eg, relative importance of gut vs. pineal-derived melatonin. Does brain melatonin talk to peripheral MT receptors? Does gut melatonin talk to brain MT receptors?
What we do know: oral melatonin works in people with circadian-related sleep disorders. This may suggest that oral/gut melatonin talks to brain MT receptors OR that oral/gut melatonin corrects circadian sleep problems by acting in the periphery. OR a major target of brain melatonin is peripheral MT receptors. I don’t know.
And as a further testament that melatonin supps aren’t sleeping pills is that they’re non-addictive and can at least temporarily “fix” circadian sleep problems: after prolonged treatment, people report no withdrawal symptoms and still sleep better even up to two weeks after discontinuation (Lemoine et al., 2011)!
In general, melatonin supps are thought to improve sleep quality, not necessarily sleep duration (although they may do that as well in some people). And poor sleep quality ruins everything. Health, cognition, well-being, quality of life -> increased risk of practically every disease, fat gain, increased risk of crashing your car… everything goes to shit.
Melatonin is the chemical expression of darkness
As for supplements, extended release is favored because it more closely mimics physiological melatonin plasma levels (regardless of whether plasma melatonin comes from brain or gut). The Lemoine study used 2 mg extended release melatonin, but other studies have shown efficacy with a range of doses. Ymmv.
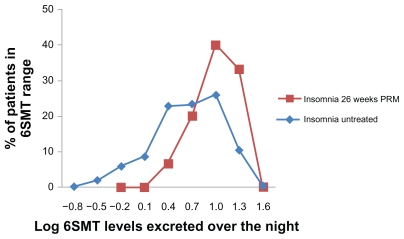
In this study, urinary 6-sulfoxymelatonin was 15ug/night in treated insomniacs, compared to 10ug in non-treated insomniacs, compared to 18ug in non-insomniacs.
“The long-term administration of PRM did not cause suppression of endogenous melatonin production as evident by the rhythm in 6SMT in the urine. The presence of such rhythm also confirms that the 6SMT was endogenous rather than a metabolite of the residual PRM discontinued 2 weeks before. The reported observations are confirmatory and compatible with earlier reports in the literature on the lack of the suppressing effect of exogenous melatonin on its endogenous production.” [seems like good news]
Tips:
Sunlight and food intake in the morning strengthens the circadian rhythm of melatonin and makes it more resilient against night time light exposure (eg, Wada et al., 2013). AND VICE VERSA: Less exposure to daily ambient light in winter increases sensitivity of melatonin to light suppression (Higuchi et al., 2007).
LED light hitting your eyes from above at night is literally the worst. If you want to read at night, try a candle at or below eye level. Or an amber bulb. And blue blockers.
This is especially important for kids: Increased sensitivity of the circadian system to light in early/mid-puberty (Crowley et al., 2015). And old people (eg, Haimov et al., 1994), who may stand to benefit more from a supp (Garfinkel et al., 1995 & Peck et al., 2004).
Sleep well.
If you like what I do and want to support it, consider becoming a Patron! Five bucks a month for full access and there are many other options. It’s ad-free and you can cancel if it sucks 🙂
Consults are open, contact me if interested: drlagakos@gmail.com.
Affiliate links: It’s 2018, join Binance and get some damn cryptoassets or download Honeyminer and get some for free!
Still looking for a pair of hot blue blockers, Carbonshade is offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE. If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.