From T.S. Wiley’s website:
“People spent summers, before electric lights, sleeping less & eating heavily in preparation for winter because the light triggered the hunger for carbohydrates. Now, light is available 24 hours a day. Heating and air-conditioning climate control our hormonal responses to consume carbohydrates now available year round. This is the scenario for obesity, Type II diabetes, and depression… In Wiley’s opinion, sleep is the best medicine.”
And Wikipedia:
“Wiley’s main thesis in Lights Out is that light is a physiological trigger that controls dopamine and hormones like cortisol. Wiley posits that with the extension of the natural day through artificial lighting, rest at the hormonal level is rarely adequate for optimum biological needs of the body. In her view, this results in both fatigue and unnatural appetite, which leads to weight gain, exhaustion, and disease. Wiley theorizes that the body’s responses are cyclical, reflecting the seasons of the year, and that the body’s needs vary seasonally. According to Wiley, during the winter months the body needs more sleep, and carbohydrates should be restricted as they would have been naturally during hunter-gatherer times.”
Most of the first third of Wiley’s book “Lights Out: Sleep, Sugar, and Survival” centers around light exposure, melatonin, and the many, many effects of a screwed up circadian cycle. Jane Plain and Jack Kruse have written volumes on the subject, please see their websites for more in-depth analyses and practical applications…
Much of this blog post is my take on that first third (I couldn’t wait to finish it before writing about it), plus a little input from Google, Pubmed, et al; some commentary & pseudo-fact-checking as well. I’m going to finish the book, and hopefully it will inspire a few more blog posts as opposed to a tin foil hat. Most of the stuff in Lights Out makes incredibly good sense, but: 1) that doesn’t mean it’s true; and 2) the strings of logic are far too long to do a proper fact-check. But really it’s how well it makes sense (mostly) that has me intrigued.
divide and conquer
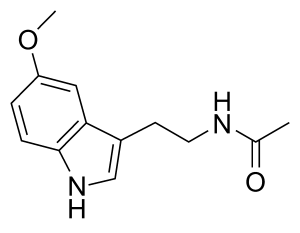
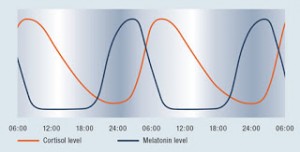
Melatonin is a sleep-inducing hormone controlled by the light-dark cycle. It is known. On the day-to-day, melatonin increases at night and decreases during the daytime. From Wiley: on a seasonal level, longer days during the summer meant less melatonin overall during these months. Since melatonin suppresses sex hormones (inconsistent? Eg, Smith et al., 2013), summer is supposed to be breeding time, so the baby is born in spring when food is plenty (I’m OK with this now, but will certainly disagree come December). Melatonin also suppresses metabolic rate, so the decreased daylight and thus increased melatonin during the winter months helped to survive on less food (supported by Marrin et al., 2013).
Disruptions in circadian rhythms royally screws us up. According to Wikipedia, fireplaces/candles and incandescent bulbs produce less of the melatonin-suppressive blue lights… use these at night in winter?
Antidepressant and circadian phase-shifting effects of light. (Lewy et al., 1987)
Abstract: Bright light can suppress nighttime melatonin production in humans, but ordinary indoor light does not have this effect. This finding suggested that bright light may have other chronobiologic effects in humans as well. Eight patients who regularly became depressed in the winter (as day length shortens) significantly improved after 1 week of exposure to bright light in the morning (but not after 1 week of bright light in the evening). The antidepressant response to morning light was accompanied by an advance (shift to an earlier time) in the onset of nighttime melatonin production. These results suggest that timing may be critical for the antidepressant effects of bright light.
Next: Prolactin inhibits sex hormones, and melatonin stimulates prolactin (supported by Gill-Sharma 2009 & Campino et al., 2008). Thus, less melatonin in summer means less prolactin = more sex & fertility. She also says day sex is more likely to result in conception compared to night sex for this reason (couldn’t find a reference for or against this).
Dopamine inhibits prolactin, whereas TRH & melatonin stimulate it. Melatonin also blunts ACTH-induced cortisol secretion (supported by Torres-Farfan 2003 & Campino 2008). Winter = high melatonin, prolactin, and low cortisol & dopamine. Summer = high dopamine & cortisol, and low melatonin & prolactin. Prolactin is supposed to be high in winter, during pregnancy; low dopamine would support this.
Dopamine is a summer hormone? Lu et al. (2006) showed high dopaminergic activity was associated with light and wakefulness (ie, summertime). However, Venero (2002) showed melatonin stimulated dopamine synthesis in specific brain regions, and Eisenberg (2010) showed increased dopamine synthesis in fall & winter relative to spring and summer. Two possible confounding factors come to mind: 1) Location, location, location! Some of these discrepancies may be due to brain region-specific dopamine metabolism… actually, Lu is the only odd-man out, so perhaps dopamine is a winter hormone? And 2) Wiley’s main premise is that we pwned the light… epigenetics and the like mean that we, including the people in those studies, have deeply screwed up light/dark summer/winter metabolic programs on an epigenetic level, so it’s possible those studies are riddles with artefacts. However, Wiley also says that people get sick because they live in perpetual summer (lights on all the time = high dopamine), and Markianos (2013) showed elevated dopamine metabolites in overweight patients; in my experience these studies usually continuously enroll patients, year-round.
I’m really just blazing through abstracts here – this is why I call it “pseudo-fact-checking;” not to be confused with any degree of academic rigor.
To be continued… (no tin foil hats, I promise) (not yet at least)
Affiliate discounts: It’s 2018, join Binance and get some damn cryptoassets or download Honeyminer and get some Bitcoins for free!
Still looking for a pair of hot blue blockers? Carbonshade is offering 15% off with the coupon code LAGAKOS and Spectra479 is offering 15% off HERE. TrueDark is running a pretty big sale HERE. If you have no idea what I’m talking about, read this then this.
20% off some delish stocks and broths from Kettle and Fire HERE.
If you want the benefits of ‘shrooms but don’t like eating them, Real Mushrooms makes great extracts. 10% off with coupon code LAGAKOS. I recommend Lion’s Mane for the brain and Reishi for everything else.