Nuts are good calories.
I’m not a big fan of the omega-6 fatty acid linoleate, but that’s largely in the context of processed foods and confectioneries, where it’s more than likely no longer in it’s native form (Dc9,1218:2n6)… but in the context of unprocessed whole foods (eg, nuts), a little n6 is fine imo.
What are good calories? They’re nutrient-dense and don’t generally lead to overeating… like the opposite of soda and junk food. Nuts are low carb and many are highly ketogenic (eg, Brazils, macadamias, and pecans are ~90%fat). Mr. Ramsey may even approve of macadamias because they have virtually zero PUFAs.
BONUS: magnesium, copper, selenium, many trace minerals and micronutrients, etc., etc.
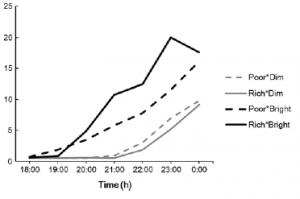
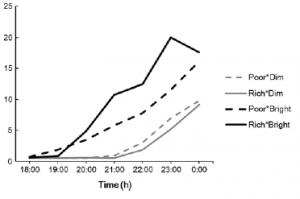
I’m not saying you should crack open a can of Deluxe Mixed Nuts and sit down with nothing to do other than NOM NOM NOM ALL THE NUTZ. I’m talking about a few nuts with a meal. Possibly earlier in the day (coinciding with LIGHT); nuts are tryptophan-rich and this may improve melatonin onset -> good for circadian rhythms:
Appetitive, dietary, and health effects of almonds consumed with meals or as snacks: a randomized controlled trial (Tan and Mattes, 2013)
In this study, the participants were instructed to eat a serving of almonds (~43g, ~245 kcal) daily for four weeks, at different times of the day (with breakfast, midmorning snack, lunch, or afternoon snack).
(~43g, ~245 kcal) daily for four weeks, at different times of the day (with breakfast, midmorning snack, lunch, or afternoon snack).
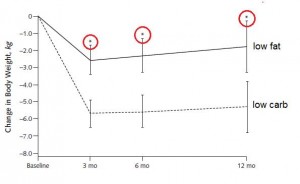
Regardless of when the almonds were consumed, the calories were practically completely compensated for. The participants unwittingly ate less other stuff. And in 3 out of 4 of the conditions, the almonds were so satiating that the participants actually ended up eating fewer overall calories.
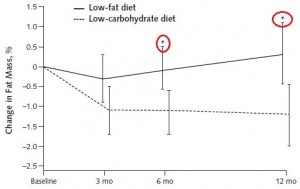
That, in a nutshell, is what I call “good calories,” and I don’t think it’s too far from Taubes’ original definition … especially because it was accompanied with [modest] reductions in body fat (NS). To be clear, they were instructed to eat more (in the form of almonds), but ended up eating less, BECAUSE ALMONDS. This wasn’t a cross-sectional study, so no healthy user bias or other obvious confounders.
… especially because it was accompanied with [modest] reductions in body fat (NS). To be clear, they were instructed to eat more (in the form of almonds), but ended up eating less, BECAUSE ALMONDS. This wasn’t a cross-sectional study, so no healthy user bias or other obvious confounders.
Further, the participants clearly weren’t obesity resistant. They were overweight, obese, or lean with a strong family history of type 2 diabetes. Sam Feltham would’ve been excluded.
This is not an isolated finding: another study showed a dose-dependent response to almonds: 28g or 42g consumed in the morning resulted in a compensatory reduction of hunger and total energy intake at lunch and dinner (Hull et al., 2014). This wouldn’t happen with soda or junk food.
Another study tested ~350 kcal almonds daily for 10 weeks and concluded: “Ten weeks of daily almond consumption did not cause a change in body weight. This was predominantly due to compensation for the energy contained in the almonds through reduced food intake from other sources” (Hollis and Mattes, 2007).
Almonds vs. complex carbs? Almonds, FTW.
1 Brazil nut daily: “After 6 months, improvements in verbal fluency and constructional praxis (two measures of cognitive performance) were significantly greater on the supplemented group when compared with the control group.” ONE FRIGGIN’ NUT !
!

Walnuts protect against alcohol-induced liver damage (in rats) (Bati et al., 2015) and may improve brain health (in humans) (Poulose et al., 2014).
protect against alcohol-induced liver damage (in rats) (Bati et al., 2015) and may improve brain health (in humans) (Poulose et al., 2014).
Pistachios improve metabolic and vascular parameters (Kasliwal et al., 2015).
Meta-analysis (not an intervention study): nut consumption is associated with lower risk of all-cause mortality (Grosso et al., 2015). Yeah yeah yeah, I know, correlation =/= causation. Whatever.
Nuts are good calories. That’s all I’m saying.
Tl;dr: buy these and one of these
and one of these , not this
, not this .
.
For personalized health consulting services: drlagakos@gmail.com
calories proper
Become a Patron!